OUR PIPELINE IS MAKING THE IMPOSSIBLE POSSIBLE
Pipeline for Rare and Common Diseases Across All Ages
An Important Update Regarding Our CAP-002 Program: A Letter to the STXBP1 Community, January 8, 2026
We have provided an update about our ongoing work to understand what happened in the SYNRGY clinical trial, which is now on clinical hold. We have been carefully examining all available information and, while we have not yet identified a root cause, we continue to investigate this unexpected and tragic event. We will share more updates with the medical and patient communities as we have more information to share.
OVERVIEW
Capsida’s pipeline consists of next generation intravenously (IV) administered gene therapies. Capsida’s gene therapies utilize proprietary engineered capsids that enable high transduction levels to desired tissues and cells, while limiting tropism to non-target organs. We have identified novel human blood-brain-barrier receptors that bind our engineered capsids. Capsida has developed IV-delivered therapeutic candidates with >70% neuronal expression and greater than 20x liver and up to 50x DRG detargeting relative to naturally occurring AAV9 in NHP studies.
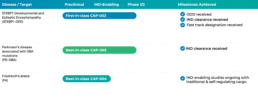
We are developing a potential first-in-class investigational therapy for STXBP1-developmental and epileptic encephalopathy (STXBP1-DEE) and potential best-in-class investigational therapy for Parkinson’s disease associated with GBA mutations (PD-GBA). We are also working on a potential best-in-class investigational therapy for Friedreich’s ataxia (FA), which is currently in IND-enabling studies and aiming to target CNS, cardiac, and sensory manifestations with a single IV infusion. For diseases of the eye, Capsida is directing its platform to engineer capsids for local delivery.
In our partnered programs we have the potential to co-develop and co-commercialize up to three CNS programs. Partnered programs target CNS and ophthalmology disease indications.
CAP-002: Capsida’s Program for STXBP1-DEE
STXBP1-DEE is a devastating developmental epileptic encephalopathy estimated to affect up to one in 26,000 births globally. STXBP1 is a protein involved in the release of neurotransmitters and neuropeptides, which are responsible for communication across neurons in the brain and throughout the central nervous system. STXBP1-DEE is characterized by early onset seizures and a risk of sudden unexpected death in epilepsy (SUDEP), severe developmental delay, intellectual disability and motor disorders. There are no disease-modifying therapies for STXBP1-DEE. Current treatments are supportive only, and include anti-seizure medication, and physical, occupational, and speech therapy.
CAP-002 is a wholly owned investigational gene therapy that is designed to stably supplement STXBP1 protein throughout the brain after a single intravenous infusion. Studies in relevant preclinical models have shown substantial detargeting of peripheral organs such as liver and dorsal root ganglia (DRG) and potential to lower dose compared to traditional gene therapy approaches. This potential disease modifying therapy aims to correct the underlying disease pathology to alleviate disease manifestations for patients with STXBP1-DEE.
CAP-002 received FDA IND clearance. The FDA has granted Fast Track and Orphan Drug Designation to CAP-002 for the potential treatment of STXBP1-DEE. More information on the Phase 1/2a SYNRGY study is available at clinicaltrials.gov (NCT06983158).
Capsida has an exclusive license agreement and research collaboration with Baylor College of Medicine and Associate Professor of Neuroscience Mingshan Xue, Ph.D., who has developed STXBP1 mouse models and AAV gene therapy approaches, in support of preclinical development of this program.
López-Rivera et al, 2020, Abramov et al, 2020, Stamberger et al, 2016, Saitsu et al., 2008; Stamberger et al., 2016
CAP-003: Capsida’s Program for PD-GBA
PD is the second most common neurodegenerative disorder, with an estimated prevalence of more than 10 million adults worldwide and nearly one million in the United States. Current evidence suggests up to 15% of PD patients have GBA1 mutations, making this the most common genetic risk factor for PD. PD involves the progressive loss of dopaminergic neurons in a part of the brain called the substantia nigra, and development and spread of aggregated protein inclusions called Lewy bodies in the brain. Patients with PD typically experience motor and non-motor symptoms, including tremor, rigidity, slowness of movement, cognitive decline, psychiatric symptoms, and sleep disturbances. PD GBA can be associated with an earlier onset and more severe disease course compared to idiopathic PD. Currently, there are no approved disease modifying treatments for any form of PD, including PD-GBA. Though standard of care is available for treatment of motor symptoms, motor fluctuations and dyskinesias (abnormal involuntary movements) develop in many patients, and non-motor symptoms will frequently persist, all of which can be debilitating in and of themselves.
CAP-003 is a next-generation systemically delivered gene therapy with best-in-class potential for the treatment of PD-GBA. This investigational gene therapy is designed to supplement GCase enzyme with a single intravenous infusion, enabling potential long-term disease modification and substantial slowing of disease progression with limited treatment burden. CAP-003 has potential for delivering GCase enzyme to critical cortical and sub-cortical areas of the brain associated with PD-GBA, such as the substantia nigra, caudate nucleus, putamen, cortex, and thalamus. Studies in relevant preclinical models have shown substantial detargeting of peripheral organs such as liver and DRG and potential to lower dose compared to traditional gene therapy approaches.
CAP-003 has received FDA IND clearance. More information on the CAP-003 Phase 1/2 study is available at clinicaltrials.gov (NCT07011771).
Smith and Schapira 2022
CAP-004: Capsida’s Program for FA
FA is a rare, hereditary, form of ataxia causing progressive neurodegeneration, decline in gait and limb control, cardiac dysfunction, and sensory deterioration. The prevalence of FA is approximately 1 in every 50,000 people, affecting approximately 5,000 patients in the US and approximately 15,000 worldwide. The average life expectancy for FA patients is 37 years of age, with death typically precipitated by cardiac dysfunction. FA is caused by an intronic triplicate repeat expansion that diminishes the expression of the frataxin (FXN) protein. FXN protein plays a critical role in cellular respiration, and in its absence, there is deficient iron-sulfur clustering in the mitochondria leading to impaired cellular respiration, oxidative stress, and cell death. Owing to eventual cell death, the impact to functions controlled by non-regenerative cell types (e.g., neurons, cardiomyocytes) is most pronounced. Currently, there are limited treatment options for FA.
CAP-004 is a wholly-owned, next generation, IV-delivered gene therapy in IND-enabling studies comprising a novel capsid designed to deliver a functional FXN gene to neurons in the CNS, cardiomyocytes, and sensory regions, thereby providing a permanent source of FXN protein allowing for restoration of cellular respiration and prevention of cell death. CAP-004 offers the potential to stably replace wild type FXN protein in disease-relevant cell types across CNS, cardiac tissues, and sensory regions with a single IV infusion. Capsida’s aim is to enable long-term disease modification across multiple organ systems and tissues impacted by the disease with limited treatment burden and provide a superior safety profile compared to traditional gene therapy. Based on CNS, cardiac and sensory targeting combined with substantial detargeting to the liver and potential for lower dosing, CAP-004 has the potential to be a best-in-class therapy that addresses significant unmet needs in FA patients.
Compassionate Use/Expanded Access Policy
We are focused on developing transformational gene therapies for people with serious diseases. We work closely with patients and families, advocacy groups, physicians, scientists, and regulators who share our commitment to advancing potential medicines to address high unmet medical needs for patients.
Access to Capsida investigational therapies is possible only through participation in carefully designed clinical trials overseen by both an Institutional Review Board (IRB) and regulatory authorities such as the U.S. Food and Drug Administration (FDA). These trials are closely monitored and regulated to help manage potential risks and are rigorously designed to evaluate safety and efficacy of our investigational therapies. The trials are critical to generate data for regulatory review and approval, with the goal of making therapies available to the broader patient population.
Our policy was established after carefully considering the potential risks and benefits of an investigational treatment, our commitment to patient safety and other ethical obligations.