UNLOCKING THE POTENTIAL OF GENE THERAPY FOR ALL
CAPSIDA APPROACH
Capsid Engineering, Cargo Optimization, Translational Biology, Process Development and Good Manufacturing Practice (GMP) Manufacturing Operations, and Clinical Development – All Under One Roof to Develop Better Therapies Faster.
Capsida Biotherapeutics is the only clinical-stage, fully integrated next-generation genetic medicine company. Capsida’s approach unlocks the potential to treat both rare and common diseases across all ages. We have three wholly owned programs.
Our investigational gene therapies for STXBP1 developmental and epileptic encephalopathy (STXBP1-DEE) and Parkinson’s disease associated with GBA mutations (PD-GBA) have received FDA Investigational New Drug (IND) clearance and we are initiating clinical trials. These are the first engineered, IV-delivered gene therapies that cross the blood-brain-barrier and detarget the liver and dorsal root ganglia (DRG) to enter clinical development.
Our third program for Friedreich’s ataxia is in IND-enabling studies and is aiming to target CNS, cardiac, and sensory manifestations with a single IV infusion.
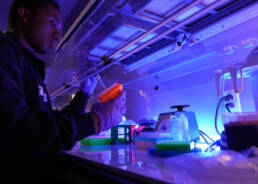
CAPSID ENGINEERING
At Capsida, the scale at which we can engineer and screen capsids is unrivaled. Using our automated, high-throughput biological screening, our scientists assess large, diverse engineered capsid libraries in models relevant to humans to quickly identify optimal capsids that target tissues and cells in organs of interest. Our customized robotics platform significantly increases throughput yielding larger data sets to improve accuracy and reproducibility to identify optimal capsids more efficiently. Our therapies are designed to achieve pre-defined disease target capsid profiles (TCPs) to target specific organs and cell types while limiting off-target tissue tropism and cell transduction. We have developed engineered capsids that transduce >70% of neurons brainwide, generating a significantly increased therapeutic index. We have identified novel human blood-brain barrier receptors that bind our engineered capsids and are conserved between primates and humans. Our, IV-delivered therapies have the potential to be administered at lower doses than wild-type AAV gene therapies, opening opportunities to pursue indications for both rare and more common diseases across all ages.
DISCOVERY AND PRECLINICAL
Capsida optimizes cargo and progresses preclinical disease proof-of-concept in parallel with capsid engineering. Our therapies can deliver a broad range of cargos including gene replacement, gene editing, gene silencing and vectorized antibodies, among others. Our R&D efforts begin by assessing the therapeutic efficacy needed to treat a given disease indication, which guides capsid engineering efforts, and then assessing candidate capsid performance in preclinical disease models, IND-enabling studies, NHPs and human disease-relevant in vitro models. Capsida’s translational research expertise allows us to define the safe and efficacious therapeutic index of a given drug product and establish clinical dosing rationale.
GOOD MANUFACTURING PRACTICES (GMP) MANUFACTURING OPERATIONS
At Capsida, we are singularly focused on rapidly getting our high-quality, life-changing therapies to patients who are suffering from debilitating diseases. We have built capabilities based on a HEK 293 platform to perform all activities in-house so that we can control the speed and quality of our development programs through pre-clinical to clinical development. This eliminates the need and the cost of contract development and manufacturing organizations (CDMOs). We start by conducting manufacturability assessments on our engineered capsids in our process development lab using our triple transfection suspension process at the 2L scale. The manufacturability assessments ensure we have high product quality and high productivity of our selected capsid/cargo candidates. Following manufacturability assessment and development candidate selection, we scale up to 50L to meet pre-clinical demand. We then transfer the process to our state-of-the-art cGMP manufacturing suite where we produce at the 200L scale for clinical trials and test the material to meet our release specifications in our quality control laboratory. As our pipeline grows, we plan on expanding our manufacturing footprint and increasing our production scale to include 500L and 1000L bioreactor capacity.
CLINICAL DEVELOPMENT
At Capsida, we are focused on improving the lives of patients. First and foremost, we approach patients holistically, working closely with clinicians, advocacy groups, patients, and caregivers to ensure we are meeting patient needs. Our highly skilled clinical development leadership and teams include medical, regulatory, and operations experts with extensive strategic and tactical experience across a wide range of adult and pediatric diseases, various treatment modalities, and innovative trial designs, with a proven track record of bringing novel medicines to market. We are excited to partner with patients, caregivers, physicians, and health authorities to bring Capsida’s differentiated gene therapies to patients.
If you are a healthcare provider who would like to get in touch with us, please send us a message at HCPs@capsida.com.
If you are a patient, advocacy group, or family member who would like to get in touch with us, please send us a message to patients@capsida.com.
EPILEPTIC ENCEPHALOPATHIES (STXBP1)

Syntaxin-binding protein 1 (STXBP1) encephalopathy is a devastating neurodevelopmental disorder affecting nearly one in 30,000 children. It is associated with severe developmental delay, treatment-resistant seizures, and early death.
STXBP1 encephalopathy is caused by mutations in the STXBP1 gene encoding a protein involved in the release of neurotransmitters and neuropeptides, which are responsible for communication across neurons in the brain and central nervous system.
There are no specific therapies for STXBP1 encephalopathy today. Treatment is supportive and includes anti-seizure medication and physical, occupational, and speech therapy to somewhat lessen the impact on daily life for patients and their families.
Capsida is developing a novel gene therapy, , for the treatment of this severe diseaseOur program is designed to stably replace STXBP1 protein throughout the brain after a single intravenous infusion, with the hope of correcting underlying pathology and significantly improving symptoms and quality of life for children with STXBP1 encephalopathy. [link to advocacy site (URL NEEDED)]
López-Rivera et al, 2020, Abramov et al, 2020, Stamberger et al, 2016, Saitsu et al., 2008; Stamberger et al., 2016
GBA-1 PARKINSON’S DISEASE

Parkinson’s disease is a brain disorder that causes unintended or uncontrollable movements, such as shaking, stiffness, and difficulty with balance and coordination. Symptoms usually begin gradually and worsen over time. As the disease progresses, people may have difficulty walking and talking. They may also have mental and behavioral changes, sleep problems, depression, memory difficulties, and fatigue.Mutations in GBA1, which encodes lysosomal enzyme glucocerebrosidase (GCase), are a relatively prevalent risk factor associated with Parkinson’s disease and aggravating disease progression. GBA1 mutations increase risk for developing PD (and related neurodegenerative disorders). PD-GBA similar to idiopathic PD, earlier onset and more rapid progression.
AMYOTROPHIC LATERAL SCLEROSIS (ALS)

Amyotrophic lateral sclerosis (ALS or Lou Gehrig’s disease) is a devastating, late-onset, neurodegenerative disease characterized by loss of both upper and lower motor neuron function. ALS affects approximately 6 in 100,000 individuals. While most cases are sporadic, familial ALS is observed in 5 to 10% of individuals who are diagnosed with ALS.
Clinically, ALS presents with focal muscle weakness, twitching or slurred speech, over time the symptoms intensify and spread to the whole body. Eventually, affected individuals lose the ability to move, chew, swallow, speak and breathe. On average, death occurs within 3 to 5 years of symptom onset.
There is no cure for ALS. Current treatments options have been shown to slow the progression of symptoms and improve quality of life but they can’t reverse the damage or stop the motor neuron demise occurring throughout the brain and spinal cord.
Capsida is developing novel gene therapy for the treatment of ALS. Delivered in a single intravenous infusion and designed to target both upper and lower motor neuron degeneration, our hope is to address the progressive loss of function and ultimately the loss of life in patients with ALS.
Mehta et al., 2018; Ajroud-Driss and Siddique 2014; ALS Association website: als.org
FRIEDREICH’S ATAXIA (FA)
Friedreich’s ataxia (FA) is a debilitating, life-shortening degenerative neuromuscular disorder affecting approximately 1 in 50,000 people. Typically, onset begins in childhood and adolescence and is characterized by progressive loss of balance and coordination and muscle weakness, leading to confinement to a wheelchair. Disease advancement is also associated speech, vision, and hearing impairment as well as heart conditions and diabetes.
Friedreich’s ataxia is caused by a defect in the frataxin gene (FXN) that leads to decreased levels of the protein frataxin. This deficiency leads to decrease cell energy production that results in the degeneration of nerve cells in the brain and spinal cord. There are no currently approved therapies to slow or reverse the disease and treatment is focused on symptom management including physical, occupational and speech therapy.
Capsida is developing a novel gene therapy for the treatment of FA. Delivered as a single intravenous infusion and targeting the underlying pathology, our aim is to alter the progression of disease and improve the quality and length of life of those affected by FA.
Zesiewicz et al; Burk et al 2017; Cook et al 2017; Zhang et al; Corben et al.